Meet Kim Updegrove. She is the Executive Director of the Mothers’ Milk Bank at Austin, and the Immediate Past President of the Human Milk Banking Association of North America. She holds Master’s degrees in both Public Health and Nursing and is a Certified Nurse Midwife. She’s an impressive lady! We wanted to chat with Kim to learn all about the in’s and out’s of the Austin Milk Bank. The Austin bank, and similar milk banks worldwide, have an ongoing and urgent need for donor milk so they can get breast milk to the smallest of our babies.
BPP: Can you give us some background on how the Mother’s Milk Bank got started and what its mission is?
KU: The mission of the Mothers’ Milk Bank at Austin (MMBA) is to save babies’ lives by providing prescribed donor human milk. Healthy lactating mothers are screened before they can donate their milk, and once approved, their milk is pasteurized, tested nutritionally and bacteriologically, and dispensed to premature and other vulnerable infants.

In 1999, two neonatologists—Dr. Sonny Rivera and the late Dr. George Sharpe—founded the Milk Bank in response to their mounting frustration at seeing premature infants who were fed formula experience serious, often fatal, complications, while those that received their mother’s milk thrived. Babies small enough to fit in your hand have a greatly increased risk of developing life-threatening conditions if fed formula, which is made of cow’s milk. The most common of these is necrotizing enterocolitis, a devastating condition causing death of intestinal tissue and subsequently a mortality rate of more than 60%. Those who survive often suffer lifelong complications as a consequence. Babies who receive only human milk feedings have a greater than 75% reduction in their risk of NEC, but mothers of babies born very early are least able to produce enough of their own milk for their babies. Donor human milk is provided when mom’s milk is unavailable.
Premature birth affects one in eight babies, and many mothers with babies in the neonatal intensive care unit (NICU) struggle to produce adequate—if any—breast milk. The stress of extended NICU stays on a mother can severely limit or even terminate milk production. That is why for the past fifteen years, the Mothers’ Milk Bank has been saving lives of preterm infants by providing more than nine million meals of donor human milk to babies whose mothers cannot provide their own. We currently serve 115 hospitals in twenty states, as well as approximately 20 outpatients in central Texas and beyond. In 2014 alone, MMBA dispensed 470,000 ounces of milk to over 2,685 babies.
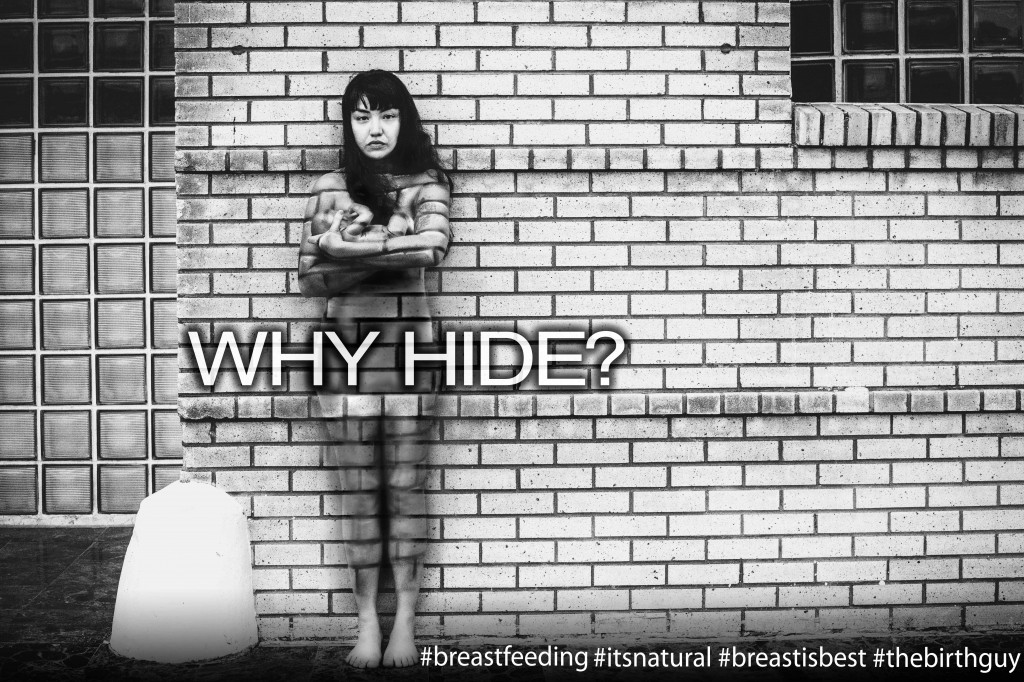
BPP: We hear the message frequently, “Breast is best.” In your own words, can you explain why breast milk is so beneficial to newborns and older babies?
KU: Breast milk is best for both infants and mothers. That’s a very simple statement to summarize a very complicated set of benefits. Babies fed breast milk receive the benefit of a species-specific food substance created just for them – meeting their nutritional, immunological, and growth needs. Breast milk-fed babies experience decreased infections, intestinal diseases, cardiovascular disease, obesity, and diabetes, to name just a few benefits. The milk changes over time reflecting the changing needs of their own bodies – in other words, it is made perfectly for them, protecting them and promoting their growth from day one, and protecting them from chronic diseases through old age. Fullterm babies need milk until at least 12 months; mothers and infants determine together whether or not it makes sense to continue beyond that first birthday. Breastfeeding is also important for the mother, as it decreases her postpartum bleeding, can help prevent another immediate pregnancy, enhances the emotional bond with her baby, burns 500 calories per day, and decreases her risks of obesity, diabetes, cardiovascular disease, and cancer.
BPP: Who qualifies to receive milk from the bank? How do they go about receiving donations?
KU: I believe that all babies deserve human milk. Not everyone chooses to breastfeed their infant, but unfortunately there isn’t enough donor milk to cover all of those infants, so milk is prioritized for the most fragile infants. Typically, this means that infants under 1500 grams, or 3 1/2 pounds, receive donor human milk until they are mature enough for a trial of formula.
Donor milk is dispensed by prescription to those with a medical need. Most of these babies are in the hospitals, but about 50 babies in homes receive milk each year as well. These babies either have continuing medical issues for which milk will help, or they are healthier babies whose physicians have written a prescription, and the milk bank’s supply of milk allowed them to receive the milk.
BPP: After someone qualifies, how do they receive the milk? Is it delivered or do they pick it up?
KU: Recipients of donor milk can be anywhere in the US, as milk is shipped frozen to the families via Federal Express. Families in the Austin area can pick up the milk directly from the milk bank.
BPP: We know that you are always looking for qualified donors and that right now you have a shortage of milk. What makes a breastfeeding mom a good candidate to be a donor?
KU: Every healthy breastfeeding mother with an infant under the age of one year could potentially save lives of infants if she would call the milk bank to be screened. The phone interview takes approximately 15 minutes, and if she appears to be an acceptable donor, she is sent paperwork to complete and return, and a lab form to take to have her blood tested. Most moms qualify and can donate milk already pumped as well as what they express and store going forward. The most common reason for not qualifying is use of medication that might be risky for a preterm infant, but moms should call and let us make that determination. The phone number is: 1.877.813.MILK (6455)
BPP: If a mom wants to donate, what is the process? Do they use their own pump? Do they drop off the milk?
KU: Moms express and store their milk in the freezer, using their own pumps or manually expressing the milk. One extra ounce pumped per day is approximately 3 meals for a preterm infant, so, literally, every drop counts. Moms in the Austin area drop off their milk at the milk bank; moms in other cities in Texas may have a milk collection site near them where they can also drop off the milk (see our website for the locations or our sites), and other moms will ship their milk to us at our expense using the coolers and Federal Express paperwork we send them.
BPP: Is the milk treated or pasteurized in any way after you receive it? How do you store your surplus?
KU: Breastmilk is a body fluid containing all of the bacteria and viruses found in our bodies. Our own babies are okay drinking our milk because they are also exposed to our immune systems and acquire our antibodies to protect them. Recipients of donor milk are foreign to us, or rather, our milk is foreign to them. Donated milk is safe for the milk bank staff to work with, but not safe for a fragile infant to drink, so the milk is heat processed in order to get rid of the viruses and bacteria we all shed in our body fluids. It is processed in a gentle way that eradicates the things that could harm a baby, while maintaining those things that the baby needs, such as fat and protein, antibodies, and growth factors. The milk is stored in freezers while awaiting final testing to verify that it is safe, and then it is sent to hospitals or outpatients. The milk is also nutritionally tested so that we can match a baby’s need with the components of the milk.
BPP: For new moms who are unable to breastfeed and do not qualify to receive donor milk from the Milk Bank, do you have any suggestions or advice on how they can provide the best possible nutrition to their newborn?
KU: Most full-term infants will be okay with some formula, so no one should beat themselves up if they cannot breastfeed. Because human milk is best for the baby, however, it is always worth a phone call to the milk bank (512-494-0800) to see if our supply is supportive of some healthier infants receiving milk. If donor milk is unavailable, and breastfeeding is not possible, the only other breast milk substitute is formula. Informal sharing of milk appears to be quite common, and yet, is not recommended because of the risks associated with sharing body fluids. Many women who feel that they cannot breastfeed could benefit from the assistance of a lactation consultant, so I encourage all who are frustrated with their efforts to seek support. (Brian the Birthguy is one of BPP’s favorites.)
BPP: Can you share a special story with us about a family that benefitted from the Milk Bank’s services?
KU: Every baby who receives donor milk is special to us, but the following story, submitted by the family, illustrates how important donor milk is to a family with an infant born at risk.
John and Sam were born at a very early 26 weeks and 4 days gestation due to Premature Rupture of Membranes (PROM). They both weighed less than 2 pounds each and were quickly issued multiple diagnoses, including Respiratory Distress Syndrome, retinopathy, osteopenia (brittle bones) and anemia.

From the outset I knew that breast milk could make all the difference, and as the situation would have it, my own production came to an abrupt end after 7 weeks. It literally pained me. How could we do our best for them without the best possible nutrition? Thankfully, St. David’s excellent NICU covered my loss with donated milk until 37 weeks, when they switched to formula and discovered that Sam was intolerant, so Sam continues receiving donor milk in our home. Having access to donated milk has saved his life, and we believe that continued availability as they’ve grown has enabled a safe passage to complete recovery for both.

John and Sam are 6.5 months old (adjusted age) now. John weighs almost 19 pounds and Sam 16.5. Both are healthy and growing with no health concerns and are happy, chatty (in syllables!) and resilient. Nobody expected this outcome less than us. We are forever grateful to the compassionate and giving-hearted mothers who played an important part in helping this come to pass. Thank you.
Many thanks to Kim for filling us in on this incredible and life-saving resource that we have here in Austin. As we mentioned earlier, they have an ongoing and urgent need for more donors, so please check out their website or give them a call (1.877.813.MILK (6455) if you have even the tiniest amount to share! C & K ♥
We also wanted to share some words from two friends of BPP who successfully donated buckets and buckets of milk to MMBA when they were breastfeeding:
Meredith O’Brien (mother to two boys) – I was blessed with an abundance of milk after having each of my children. I had so much milk that it was really uncomfortable, and I was having to pump 2-3 times a day in addition to feeding my hungry baby. At first I would dump the milk down the drain, but then somewhere, from someone (probably some random mom at a jumpy gym) I heard about Austin’s Mother’s Milk Bank.
I called the Milk Bank and said I’d like to be a donor. They were very glad to hear from me, and asked if I’d like to come tour the facility. I put Timmy in the BabyBjorn and headed over. I was given a comprehensive tour of the milk bank, and was amazed at how organized the process it was. They showed me where all the milk is stored and how it is tested. They explained to whom my milk would go, how it would get there, and how appreciated it would be. Naively, due to my clear privilege, I never realized how many babies are born to mothers who are unable to nurse, be it due to a lack of milk, or drugs, or many other reasons. The overwhelming feeling I got from the Mother’s Milk Bank was how appreciative they were of my willingness to donate. I told them it was a two way street — I was pumping so much out of a need for physical relief. What I felt after I started to donate was an incredible sense of emotional relief. I was helping babies! I was helping their parents! It felt really good on so many levels. I would fill up my freezer with bags of milk clipped shut with a little pink clip — probably four – five bags a day at least. We didn’t have room in the freezer for ice cream!
My one issue, I told the people at the Milk Bank, was transporting the milk to the bank. I felt overextended with my activities at home, and wasn’t sure how I would get the milk to the Bank every week. They immediately enlisted the aid of a Junior League member who would come to my home at the end of each week with a large igloo cooler, collect the frozen bags of milk, and take it to the facility. She was a Godsend.
My entire experience of donating breast milk, from beginning to end, was positive and fulfilling. And easy! I’m so glad that places like this exist in the world — it makes me feel like things really do work out if we work together.
Linda Classen (mother to a boy and girl) – I enjoyed donating to the Milk Bank. It was very rewarding because I knew babies were going to benefit from my milk. I was fortunate enough to be able to produce enough milk to share with other babies.
Thank you for sharing your experiences ladies. You two rock and we’re sure that many premature babies benefited!